Current treatment and disposal practices for medical wastes in Bujumbura, Burundi
Article information
Abstract
Since improper management practices of solid medical waste (SMW) could potentially result in serious health risks and environmental problems, it is very important to properly treat and dispose of the medical wastes. In this study, current practices of SMW management from storage to final disposal stage in 12 health care facilities (HCFs) of Burundi were investigated using the official government reports. The results showed that 75% and 92% of HCFs used uncovered wheelbarrows and trucks for on-site or off-site SMW transportation, respectively, indicating that most transportation equipment and waste workers are not safely protected. The results also showed that 92.8% of SMW (15,736.4 ton) from all 12 HCFs were inappropriately disposed of through uncontrolled land disposal and incineration. If pharmaceutical wastes and discarded medical plastics (29.5% of SMW) can be separated and treated properly, the treatment costs can be reduced and resource savings can be achieved. Raising awareness of healthcare workers and general public about potential health effects arising from improper SMW management, sufficient financial and human resources for the treatment facilities (especially incinerators), and effective regulations and guidelines for transportation and treatment of SWM are some of the major tasks for safe and sustainable medical waste management in Burundi.
1. Introduction
Solid medical waste (SMW) is generated during various medical services such as diagnosis, treatment or immunization. It often contains potentially infectious or toxic materials. It, therefore, should be clearly identified and safely collected, separated at the source, and properly treated to minimize any potential risks that would result during the management processes [1–3]. For example, a number of groups such as healthcare workers (particularly nurses), patients, hospital housekeeping personnel, visitors to health care facilities (HCFs), or even public in the community via direct or indirect exposure pathways can be exposed to or infected by potentially infectious and harmful microorganisms in the waste.
Potential health and environmental threats have led many developed countries to establish and implement proper management measures to manage medical wastes. Relevant legislations have been enacted and strengthened and new treatment technologies have been developed to safely dispose of medical wastes. Efforts have been made to reduce the negative environmental impacts that could occur during final disposal [4]. For example, the Medical Waste Tracking Act (MWTA) was passed in 1988 after improper handled medical wastes were frequently found on beaches and then the US Environmental Protection Agency has developed technologies to safely treat medical wastes. Incineration has become the most common method of final disposal of medical wastes and stricter emission standards have been implemented [4]. As a result, a number of safer technologies such as incineration, steam sterilization, microwave sanitation, chemical disinfection, dry heat disinfection, and disinfection with superheated steam have now been used in medical waste treatment in developed countries. As part of pretreatment, autoclaves, microwaves, chemical disinfection and mechanical destroyer are used to reduce risk by disinfection of infectious wastes or shredding the sharps wastes [3–6]. Uncontrolled land disposal of SMW is not generally accepted in many countries by legislations and regulations. There are stricter controls of landfilling of wastes and public resistance to land disposal due to its environmental impacts. Disposing of medical wastes in sanitary landfills (controlled and engineer-designed landfills) is widely unacceptable in industrialized countries partly because it is typically considered as hazardous wastes.
However, the status of medical waste disposal in developing countries still has many problems. SMW was mixed during collection or storage steps and disposed of at the municipal dumpsites without pretreatment in Nigeria. Some are burned in the incinerators that had insufficient capacity and operated without adequate protection to the human health and environment [7, 8]. General and medical wastes from two HCFs in South Africa were disposed of at an open dumping site near the hospitals and residential area without separation. Some medical waste is still dumped at open dumping sites in Lybia and Ghana. The absence of guidelines related to the appropriate management and practices of medical wastes was the main problem in both countries [2, 9]. WHO estimated that injections with contaminated syringes caused 21 million hepatitis B, 2 million hepatitis C and 260,000 HIV infection [10].
The main reason for the mismanagement of SMW in developing countries is that the governments do not have adequate knowledge of the risks posed by medical wastes and they lack proper waste disposal systems [11]. Many developing countries do not have any legislation on medical wastes, and even if they do, they are not properly implemented [4]. Due to lack of financial support and interest from the government, it is extremely difficult for those countries to introduce new technologies such as environmentally friendly incinerators and safely manage SMW [12–16]. Therefore, safe transportation, treatment and disposal of SMW in developing countries have received much attention of international communities in recent years. Development of an effective SMW management is crucial for the prevention of the potential exposure of healthcare service workers, patients, and the public to infections, toxic chemicals, and accidental hazards as well as the protection of the environment [4, 17]. Previous studies in Burundi have shown that most SMW was not managed safely inside HCFs and the risk of exposure to hazardous SMW for patients, medical teams, and workers inside the facilities was high. If those mismanaged SMW still have problems in subsequent storage and final disposal stage, they can pose a high risk to waste handlers, workers in waste treatment and disposal facilities, and general public, and result in other environmental problems such as drinking water pollution, rodent and pest growth, unpleasant odor, and soil and groundwater contamination [18, 19]. However, there is no national guideline for final treatment and disposal of SMW and no information on SMW management status from transportation to the final treatment or disposal sites. Therefore, this study attempts to quantitatively assess the current practices of medical waste management in a poor developing country, Burundi, which does not have enough financial and technological capability. This study aims to assess the current status of transport and final disposal of SMW in Burundi, to identify the type of waste threat, and to present their impacts on the ecosystem and human society. The results of this study could contribute to raising the awareness of the Burundi government, medical staff, and general public on the risks associated with improper medical waste disposal, encouraging the Burundian government to improve the SMW management policies and their administration and adopt appropriate technologies at each stage of medical waste disposal.
2. Materials and Methods
2.1. Study Area
To investigate status of SMW transport and final disposal, twelve HCFs were selected among fifteen HCFs with inpatient wards in Bujumbura, Burundi, taking into account the location of HCFs and their operation levels. Bujumbura has three districts with a total area of 11,000 km2. Four HCFs are located in north district, 7 in central district, and 1 in south district (Fig. 1). The populations of the northern, central and southern districts in 2008 were 187,046, 172,120, and 138,000, respectively. The average temperature is 23°C and annual precipitation is 1,274 mm. Burundi’s gross domestic product (GDP) per capita in 2017 is $ 343.39, ranking 187th in the world. Current Health Expenditure per Capita is $ 24 in 2015 and health capital expenditure is less than 1% of GDP [20–22].
2.2. Data Collection and Analysis
Current practice data on generation, transport and final disposal of SMW were collected from the official government report prepared by the Ministry of Health (MOH) of Burundi [23]. Each HCF measured daily SMW production, completed a government-distributed questionnaire, and produced a monthly report under the supervision of the district offices that are involved in the management of SMW. The MOH of Burundi investigated monthly report and produced an annual report. Burundi has national guidelines for transporting SMW only, but not for final disposal [24]. Therefore, the adequacy of the transport phase was assessed by whether the HCFs followed the national guidelines or not. The guideline for SMW transport in Burundi consists of three components; safe transport equipment (use of covered trucks and wheelbarrows), protection of waste workers, and regular transportation [24]. The appropriateness of the final treatment stage was also assessed by comparing current treatment methods with the WHO recommendations [3, 10]. The generation characteristics of SMW in 12 HCFs during 2011–2014 were analyzed using descriptive statistics. Daily SMW generation rates per patient and per bed were calculated using the number of patients and beds with total SMW generation in each HCF. The current practice of transporting and disposing of SMW in HCFs has also been analyzed using the questionnaire report. After evaluating the compliance with the national guideline in each management stage and whether appropriate treatment methods were applied for each SMW type, the throughputs at each stage and for SMW types were calculated and then the amount of SMWs incorrectly treated for each type of waste in 12 HCFs has been estimated.
3. Results and Discussion
3.1. Generation Characteristics of SMW in 12 HCFs
A total of 16,959 tons of SMW were generated during 2011–2014 in 12 HCFs in Bujumbura, Burundi. Generation rates per patient and bed are 0.27 ± 0.17 kg/patient/d and 4.13 ± 3.55 kg/bed/d, respectively. Public HCFs generated 93% (15,437 ton) of SMW (Fig. 2(a)) because free care was provided in public HCFs to pregnant women, AIDS patients, and children under the age of five years [25]. In terms of districts, the central district produced the most SMW comprising 61% (10,304 ton) of SMW. The north district generated 38% (6,509 ton) and the south district only 1% (146 ton) (Fig. 2(b)). With regard to the type of SMW generated, pathological waste and tissue were the most abundant SMW accounting for 37.9%, followed by pharmaceutical wastes and discarded medical plastics (27.4%) and infectious waste and absorbent cotton (19.6%), medical sharps (9.3%), and chemical waste and radioactive waste (5.5%). Placenta only occupied 0.25% of the total (Fig. 2(c)).
3.2. Current Practices of SMW from Storage to Final Disposal in 12 HCFs
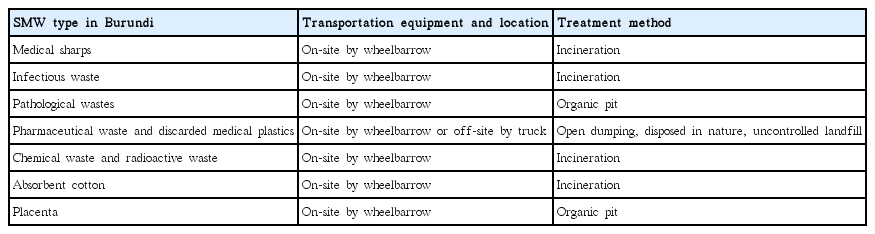
The current management practices for transportation and final treatment of SMW in 12 HCFs in Bujumbura, Burundi, are presented in Fig. 3. After temporary storage of SMW in a designated storage area at HCFs, SMW can be disposed of at on-site facilities or should be transported to off-site treatment facilities. When SMW is transported, it should be collected regularly using closed or covered transport equipment and waste handlers should be safely protected [3]. The waste materials were transported from storage areas to either on-site disposal facilities by wheelbarrows or off-site disposal sites by trucks in 12 HCFs. Table 1 shows treatment methods and transportation equipment for each type of SMW currently used in 12 HCFs in Bujumbura, Burundi.
Current practices of SMW management in 12 HCFs from storage to final treatment in Bujumbura, Burundi.
The HCFs that followed the current practices and the amount of wastes that were not properly handled during the transportation process are presented in Fig. 4. Pharmaceutical wastes and disposable medical plastics have been reported to dispose at on-site dumping sites or off-site uncontrolled landfills. However, since it is not known for some HCFs how much SMW are disposed of inside HCFs, this study assumed that all pharmaceutical wastes and disused medical plastics are disposed of at off-site landfills and transported using trucks. The results showed that most of trucks used for transportation of 70.8% (3,292.2 ton) of pharmaceutical wastes and discarded medical plastics from storage areas to off-site uncontrolled landfills were not properly protected (Fig. 4). People could be potentially exposed to those wastes if they contain any cytotoxic or infectious wastes by inappropriate separation.
Other SMWs treated by on-site incinerators or organic pits were transported using wheelbarrows. However, 75% of HCFs used uncovered wheelbarrows and 7,850.1 tons of SMW were not transported appropriately. During on-site SMW transportation, waste workers in 67% of HCFs that are 92 out of 130 workers were not safely protected during 2011–2014. Because SMW can be infectious, radioactive or toxic, not only workers but also the staff members in HCFs are potentially exposed to them during normal work or by accidental hazards. Waste handlers are more exposed to potential risks associated with other diseases through direct contact [26]. The safety status of the SMW transport stage in other developing countries is similar to that in Burundi. Transportation of stored SMW to final disposal sites is irregular and transportation vehicles pass through residential areas without a cover in Libya [2]. Guidelines of off-site transportation, during which SMW is most likely to be exposed to the environment and humans, are not being followed properly in Uganda and Cameroon [27, 28]. There are no relevant national policies and guidelines, and even transportation equipment is in very poor conditions, leading to a high possibility of exposure to the people during transportation [13]. Another problem during the transportation process is that SMW can be transported together with general wastes. Developing countries in Asia, such as Cambodia and Myanmar, also share the problem because same transportation vehicles and equipment are used for both general wastes and SMW [29].
Another problem with SMW transportation is that the SMW in the storage area is not transported on a regular basis. If the SMW is not removed regularly and stored beyond a period recommended by the guideline, the waste may decompose and produce unwanted odor or cross-contaminate through mixing of wastes due to lack of space especially during the hot season [3]. Current vehicles used in Bujumbura, Burundi, to transport SMW can increase the health and environmental risks because they lack necessary safety measures. In this study, however, only HCF1 transported SMW from storage area to final disposal site regularly. Approximately 69.1% (11,724 ton) of SMW were placed in storage area for longer than the recommended period in the guideline (Fig. 4). Since Burundi’s waste storage facilities are constructed without enough safety measures implemented, secondary contamination by the waste is also an issue of concern.
Improvement of transportation system of SMW in HCFs is important. Safe transport of SMW inside HCFs is the responsibility of the facilities. Proper equipment needs to be supplemented. Because unsafe transportation of SMW results from lack of understanding of the current guideline, the current guideline should be revised in such a way that all the personnel involved in the transportation process can easily understand the proper procedure and a better training program for workers needs to be implemented. Although it is essential to strengthen the internal waste management for regular SMW transfer, consideration should also be given to the outsourcing of SMW transport for off-site treatment. In some countries such as Iran and South Africa, off-site transportation is carried out by municipalities [30, 31].
3.3. Final Treatment of SMW in 12 HCFs
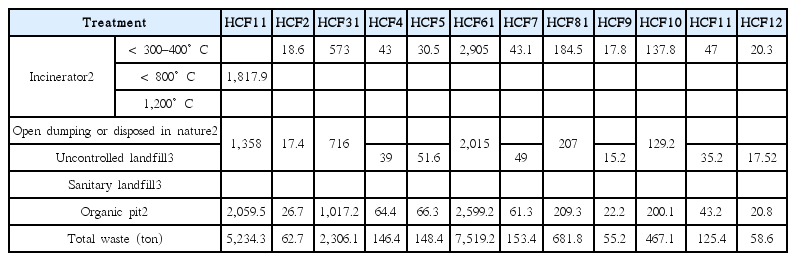
The infectious wastes, medical sharps, chemical wastes, radioactive wastes and absorbent cotton were treated by incinerators at low (< 300–400°C) or medium temperature (< 800°C) in the HCFs (Table 2). Table 3 shows the estimated amount of SMW treated by each final disposal method by 12 HCFs in Bujumbura, Burundi. On-site incineration was performed in all 12 HCFs. Low temperature incinerators constructed with burnt bricks and cement are poorly designed and have insufficient capacity (Fig. 5). About 23.8% (4,020.6 ton) of SMW produced during 2011–2014 was treated by the low temperature incinerators (300–400°C) in 11 HCFs. However, the incineration capacity and the treatment temperature are insufficient to complete the incineration of SMW and may produce harmful gases such as dioxins and furans during the incineration process [32, 33]. A total of 1,817.9 tons of SMW (10.7%) were incinerated from HCF1 using a medium temperature incinerator (Table 2). Medical sharps, chemical wastes, and radioactive wastes should be treated securely with different methods. Most incinerators are located only 15 to 30 meters from the residential area and do not have facilities to handle the exhaust gas [25]. The incineration of these substances may release harmful substances during incineration and may affect the health of not only waste workers but also nearby residents. Improper incineration is not a problem in Burundi alone. HCFs in other African countries such as Limpopo province in South Africa, Uganda and Egypt used low temperature incinerators made from cement and bricks [6, 27, 34].

Incinerators used to treat solid medical wastes in 12 HCFs in Bujumbura, Burundi. (a) Low temperature incinerator and (b) Medium temperature incinerator.
Pharmaceutical wastes and discarded medical plastics were disposed of in nature or at open dumping sites in HCFs (Fig. 6(a)) and burned irregularly or treated at off-site uncontrolled landfills (Fig. 6(b)). However, half the HCFs including all the public HCFs did not record how much waste was disposed of at the uncontrolled landfills (Table 2). Public HCFs were responsible for 95.5% of pharmaceutical wastes and discarded medical plastics buried at open dumping sites and landfills (Table 2). In the hospitals of Lybia, Ghana and Limpopo Province of South Africa, SMWs are still dumped at uncontrolled landfills as in Burundi [2, 6, 13].

Types of burial of SMW used by 12 HCFs in Bujumbura, Burundi (a) open dumping (on-site), (b) uncontrolled landfills (off-site), and (c) organic pit (on-site).
As a result, 27.48% of SMW were disposed of at open dumping sites or uncontrolled landfills. A total of 34.4% of SMW were incinerated without proper emission control. If SMW continues to be improperly treated at landfills and by incinerators, soil, surface water, ground water and air in adjacent areas may be contaminated by toxic substances or infectious pathogenic microorganisms. Humans and animals can be exposed to pollutants through a variety of routes such as skin contact and penetration, inhalation and ingestion through the food chain [3, 35]. Animals, insects and birds could be affected by hazardous wastes, while they could become vectors that transmit pollutants or germs.
In developing countries, most SMW were not separated properly and were treated by incinerators with insufficient capacity and temperature or dumped at uncontrolled landfills [13, 27, 36]. In Cameroon, only 4 out of 30 hospitals used low-temperature incinerators and the rest disposed of SMW using dumping pits. The commonly used disposal methods in Aba, Nigeria, are landfilling at open dumpsites [37]. The problem is that these dumpsites are not protected and thus waste pickers and animals can enter them freely [27, 28].
Organic pits were used to dispose of pathological wastes and placenta (Fig. 6(c)), accounting for the disposal of 38.16% (6,390.2 ton) of SMW generated during 2011–2014 in 12 HCFs. Organic pits in four public HCFs treated 5,885.2 tons of SMW. Although organic pits are one of recommended methods by WHO for placenta, pathological wastes should be treated by other safe methods such as incineration [3, 38]. SMW treatment in Ethiopia is similar to that in Burundi in that placenta is treated separately in placenta dumping pits [16]. However, organic pits currently in use in Burundi must be supplemented with safety devices such as roofs and fences [3].
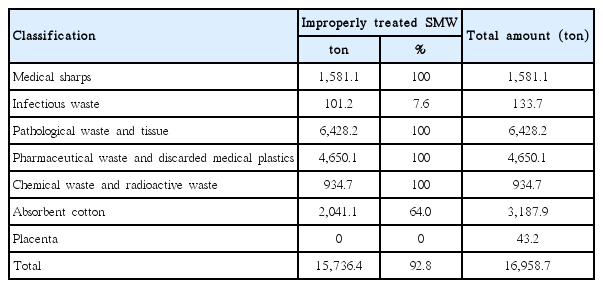
The quantity of SMW improperly treated in 12 HCFs during four years (2011–2014) is presented in Table 3. The results show that a total of 15,736.4 tons (92.8%) were inappropriately treated in the HCFs of Bujumbura, Burundi. The present treatment methods for medical sharps, pathological wastes, infectious wastes and absorbent cotton should be improved. Medical sharps may be processed in low temperature incinerators in other developing countries [36], but it is not safe method. Sharp wastes should be disinfected or destroyed and separately disposed of using sharps pits or encapsulation. This can reduce 10% of SMW that is improperly treated. Incinerating medical sharps can affect the incineration of other SMW because the capacity of the incinerator is not sufficient at present. It can also have a negative impact on the complete combustion of wastes such as infectious or absorbent cotton that are mostly treated at low temperature incinerators. Therefore, it is not appropriate to use incinerators to treat sharps even though incineration can act as a pretreatment for final disposal of medical sharps.
Pathological wastes should be completely incinerated, not disposed of using organic pits as currently practiced in Bujumbura, Burundi. Because they are the most produced SMW in 12 HCFs, storage space problems could occur within a short period of time. The capacity of organic pits in all the HCFs was relatively small (30–54 m3), and they were built without much safety consideration [29]. It can overflow due to rain and floods or leachate can contaminate soil and groundwater. In both cases, it can pose a serious risk to people and the environment. Because of such shortcomings, WHO recommends that HCFs first use a high temperature incinerator and an engineered organic pit, if it is unavoidable [3, 10].
Pharmaceutical wastes and discarded medical plastics should be separated. The former should be returned to the manufacturer, encapsulated, buried at a sanitary landfill or incinerated at high temperature, while the latter can be recycled. If pharmaceutical wastes and disused medical plastics (4,650.1 tons) that account for 29.5% of the total SMW were properly disposed of, the treatment costs could be reduced and resources saved depending on the degree of recycling. Chemical wastes and radioactive wastes should be carefully managed. They are currently being incinerated, but they should be sent back to supplier or safely disposed of. Radioactive wastes should not be incinerated as it is currently practiced [3]. Only placenta was disposed of safely, but it is necessary to supplement safety facilities as mentioned above. Since placenta is of great value for medical uses, it is not desirable to simply discard it.
If enough capacity of incinerators is available to treat SMW at medium or high temperature, a total of 8,570.5 tons of infectious wastes, absorbent cotton and pathological wastes can be treated safely. They comprise 54.4% of inappropriately disposed SMW in 12 HCFs in Bujumbura, Burundi. However, incineration has also some disadvantages, including the potential emission of toxic substances into the surrounding area, high operation and maintenance costs, and the requirement of ash disposal. There is a great potential for emission of toxic air pollutants from medical waste incinerators, if improperly operated and managed, partly because it typically contains a variety of plastic materials (e.g., polyvinyl chloride) as well as toxic materials. Emissions from medical waste incinerators may include carbon monoxide (as a result of incomplete combustion), particulate matter, hydrogen chloride, metals (e.g., mercury, lead, arsenic, and cadmium), polycyclic aromatic hydrocarbons (PAHs), and dioxins (polychloro-dibenzo-p-dioxin (PCDD)) and furans (polychloro-dibenzo-furan (PCDF)) that are carcinogens [3].
Many air pollutants in emissions from medical waste incinerators can be significantly reduced by modern air pollution control devices if properly designed and operated. Typical air pollution control devices used for medical waste incinerators in developed countries may include cyclones, semi-dry scrubbers, and bag house filters (or fabric dust removers). Many devices can be modified to effectively control dioxins and furans. Therefore, when installing an incinerator, it is necessary to provide a safe distance from residential areas, equip with a hazardous gas treatment facility, and prepare measures to safely treat the ash.
Table 4 describes potential threats to human and ecosystems that could occur if the current transportation system and final disposal method were to be continued. Regardless of inside or outside the hospital, all persons and ecosystems exposed to the transport or treatment route of SMW are at greater risk of exposure to hazardous waste and can be directly or indirectly a potential victim. Therefore, it is imperative that integrated management and an improvement in the final disposal system of SMW in Burundi are needed.
More specifically, improvement of the entire SMW treatment system is required in accordance with WHO recommendations, as in the developed countries such as the United States, the EU, the United Kingdom, Australia, Canada, and Korea that use high temperature incinerators, sanitary landfills, and recycling [8, 38, 39]. In order to improve the waste management in developing countries, it is necessary to improve education and awareness, to develop suitable technologies and to increase investment [37]. However, considering Burundi’s low economic status and poor medical sector investment, it seems difficult to improve SMW treatment system immediately. The lack of budget and absence of guideline for final treatment were the main reasons that the majority of HCFs used the low temperature incinerators in Burundi [25]. Therefore, if financial investment is difficult, improvement of regulations and guidelines as well as education and training of medical personnel should be preceded. Establishment of proper management policies for SMW is not possible without objective and reliable data for every stage of SMW management. A quality control system for data collection on SMW needs to be a top priority for the Burundian government to improve SMW management.
3.4. Practical Suggestions
Inappropriate management of SMW could result in serious health and ecological hazards during transit from storage to treatment facilities as well as final disposal in Burundi. The followings are recommendations to the Burundi government to improve SMW management of the country.
Safe transportation equipment needs to be supplemented and the current guideline should be revised.
Proper pretreatment should be introduced to reduce volume and potential risks of SMW.
Safe treatment should be considered first, but source separation system that can segregate unpolluted or infection-free recyclable SMW should be improved together.
Pharmaceutical wastes and discarded medical plastics should be separated. The former should be returned to the manufacturer, encapsulated, buried at a sanitary landfill or incinerated at high temperature, while the latter can be recycled.
Medium or high temperature incineration should be employed to handle SMW that contains potentially infectious and toxic materials, but should be located at a safe distance from residential areas, and equipped with air pollution prevention system.
Uncontrolled land disposal of SMW should be prohibited by legislations and regulations.
Sharp wastes should be disinfected or destroyed and separately disposed of using sharps pits or encapsulation.
Pathological wastes should be completely incinerated, not disposed of using organic pits.
Chemical wastes and radioactive wastes should be carefully managed and should be sent back to supplier or safely disposed of.
Organic pits currently in use in Burundi must be supplemented with safety devices such as roofs and fences.
4. Conclusions
Since improper management practices of SMW could potentially result in serious health risks and environmental problems (e.g., the spread of infectious diseases, direct/indirect human exposure to toxic materials), it is extremely important to properly treat and dispose of the waste. In this study, the transportation and final disposal of SMW in Bujumbura, Burundi, was evaluated based on data collected from 12 HCFs. The results showed that most transportation equipment as well as workers was not safely protected. Approximately 75% (7,850 ton) and 92% (3,292 ton) of HCFs used uncovered wheelbarrows and trucks for on-site and off-site SMW transportation, respectively, exposing healthcare workers or the public to potential risks. To make matters worse, 67% of HCFs that are 92 out of 130 workers were not safely protected during 2011–2014. Only HCF1 transported SMW from storage area to final disposal site regularly. About 69.1% (11,724 ton) of SMW were placed in the storage area for a long period of time. Transportation system of SMW with proper equipment in Burundi should be improved.
The results also showed that 92.8% (15,736.4 ton) of SMW were inappropriately treated in all the HCFs of Bujumbura, Burundi. The present treatment method for medical sharps, pathological wastes, infectious wastes and absorbent should be improved. If sufficient capacity of medium or high temperature incinerators is available to treat SMW, 54.4% (8,570.5 ton) of infectious wastes, absorbent cotton and pathological wastes can be safely treated.
In Burundi, recycling may be dangerous and inadequate because there is no pre-treatment of SMW and poor separation of SMW. Only metal medical sharps were collected and recycled after incineration, but no other SMW has been recycled. Among SMW produced in Bujumbura, Burundi, discarded medical plastics are recyclable wastes. However, in order to recycle the plastics, separation must be ensured, and if contaminated, pretreatment is also necessary. Appropriate recycling has a positive impact on the environment and may also generate economic benefits by reducing the amount of waste generated and the waste of reusable resources. If pharmaceutical wastes and discarded medical plastics (29.5% of SMW) can be separated and recycled, the treatment costs can be reduced and resource savings can be achieved.
Based on the results of this study, lack of awareness of healthcare workers and general public about potential health effects arising from medical wastes, insufficient financial and human resources for proper treatment like advanced incineration technology, and ineffective legislation and regulations for SMW seem to be the major barriers to manage medical wastes in Burundi safely and sustainably. Proper transportation with controlled equipment and the control of toxic air emissions from medical waste incinerators and alternative treatment methods to open dumping are the major future challenges for waste management professionals and HCFs in Burundi.
Acknowledgments
This work was supported by a Research Grant of Pukyong National University (2016 year). We thank Ndizeye Aloys and Mpawenimana Juvenal in Ministry of Health of Burundi for providing data information.